不良反应有头晕、嗜睡等症状,药效过后可自行消失患者不必惊慌;大剂量服药时可能会出现呼吸道阻塞的情况。
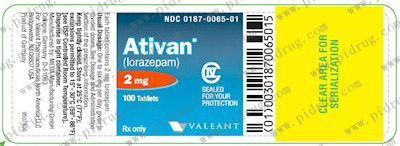
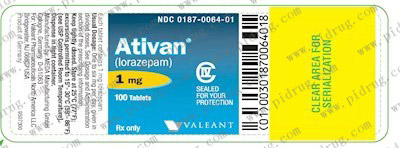
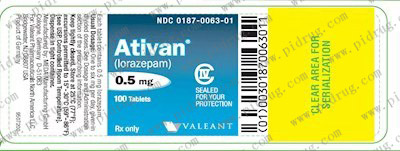
Ativan(Lorazepam)
Lorazepam, sold under the brand name Ativan among others, is a benzodiazepine medication.[3] It is used to treat anxiety disorders, trouble sleeping, active seizures including status epilepticus, alcohol withdrawal, and chemotherapy-induced nausea and vomiting.[3] It is also used during surgery to interfere with memory formation and to sedate those who are being mechanically ventilated.[3][7] While it can be used for severe agitation, midazolam is usually preferred.[3] It is also used, along with other treatments, for acute coronary syndrome due to cocaine use.[3] It can be given by mouth or as an injection into a muscle or vein.[3] When given by injection onset of effects is between one and thirty minutes and effects last for up to a day.[3]
Common side effects include weakness, sleepiness, low blood pressure, and a decreased effort to breathe.[3] When given intravenously the person should be closely monitored.[3]Among those who are depressed there may be an increased risk of suicide.[3][8] With long-term use, larger doses may be required for the same effect.[3] Physical dependence and psychological dependence may also occur.[3] If stopped suddenly after long-term use, benzodiazepine withdrawal syndrome may occur.[3] Older people more often develop adverse effects.[9] In this age group lorazepam is associated with falls and hip fractures.[10]Due to these concerns, lorazepam use is generally only recommended for up to two to four weeks.[11]
Lorazepam was initially patented in 1963 and went on sale in the United States in 1977.[12] It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system.[13] It is available as a generic medication.[3] The wholesale cost in the developing world of a typical dose by mouth is between US$0.02 and US$0.16 as of 2014.[14] In the United States as of 2015 a typical month's supply is less than US$25.[15] In 2016 it was the 57th most prescribed medication in the United States with more than 14 million prescriptions.[16]
Medical uses
Anxiety
Lorazepam has anxiety-reducing effects and its best-known indication is the short-term management of severe anxiety. In the US, the FDA advises against use of benzodiazepines such as lorazepam for longer than four weeks.[11][17] It is fast acting, and useful in treating fast onset panic anxiety.[18]
Lorazepam can effectively reduce agitation and induce sleep, and the duration of effects from a single dose makes it an appropriate choice for the short-term treatment of insomnia, especially in the presence of severe anxiety or night terrors. It has a fairly short duration of action.[19]
Withdrawal symptoms, including rebound insomnia and rebound anxiety, may occur after seven days' use of lorazepam.[20]
Seizures
Intravenous diazepam or lorazepam are first-line treatments for convulsive status epilepticus.[21][21] Lorazepam is more effective than diazepam and intravenous phenytoin in the treatment of status epilepticus and has a lower risk of continuing seizure that might require additional medication.[22] However, phenobarbital has a superior success rate compared to lorazepam and other drugs, at least in the elderly.[23][24]
Lorazepam's anticonvulsant properties and pharmacokinetic profile, make intravenous use reliable for terminating acute seizures, but induces prolonged sedation. Oral benzodiazepines, including lorazepam are occasionally used as long-term prophylactictreatment of resistant absence seizures; because of gradual tolerance to their anti-seizure effects, benzodiazepines such as lorazepam are not considered first-line therapies.[25]
Lorazepam's anticonvulsant and CNS depressant properties are useful for the treatment and prevention of alcohol withdrawal syndrome. In this setting, impaired liver function is not a hazard with lorazepam, since lorazepam does not require oxidation, hepatic or otherwise, for its metabolism.[26][27]
Sedation
Lorazepam is sometimes used for individuals receiving mechanical ventilation. However, in critically ill people, propofol has been found to be superior to lorazepam both in effectiveness and overall cost; as a result, the use of propofol for this indication is now encouraged, whereas the use of lorazepam is discouraged.[28]
Its relative effectiveness in preventing new memory formation,[29] along with its ability to reduce agitation and anxiety, makes lorazepam useful as premedication. It is given before a general anesthetic to reduce the amount of anesthetic required, or before unpleasant awake procedures, such as in dentistry or endoscopies, to reduce anxiety, to increase compliance, and to induce amnesia for the procedure. Lorazepam by mouth is given 90 to 120 minutes before procedures, and intravenous lorazepam as late as 10 minutes before procedures.[30][31][32] Lorazepam is sometimes used as an alternative to midazolam in palliative sedation.[33] In intensive care units lorazepam is sometimes used to produce anxiolysis, hypnosis, and amnesia.[34]
Agitation
Lorazepam is sometimes used as an alternative to haloperidol when there is the need for rapid sedation of violent or agitated individuals,[35][36] but haloperidol plus promethazine is preferred due to better effectiveness and due to lorazepam's adverse effects on respiratory function.[37] However, adverse effects such as behavioral disinhibition may make benzodiazepines inappropriate for some acutely psychotic patients.[38] Acute delirium is sometimes treated with lorazepam, but as it can cause paradoxical effects, it is preferably given together with haloperidol.[39] Lorazepam is absorbed relatively slowly if given intramuscularly, a common route in restraint situations.
Other
Catatonia with inability to speak is responsive to lorazepam. Symptoms may recur and treatment for some days may be necessary. Catatonia due to abrupt or overly rapid withdrawal from benzodiazepines, as part of the benzodiazepine withdrawal syndrome, should also respond to lorazepam treatment.[40] As lorazepam can have paradoxical effects, haloperidol is sometimes given at the same time.[39][41]
It is sometimes used in chemotherapy in addition to medications used to treat nausea and vomiting, i.e. nausea and vomiting caused or worsened by psychological sensitization to the thought of being sick.[42] It is also used as adjunct therapy for cyclic vomiting syndrome.
Contraindications
Lorazepam should be avoided in people with:
Allergy or hypersensitivity – Past hypersensitivity or allergy to lorazepam, to any benzodiazepine, or to any of the ingredients in lorazepam tablets or injections
Severe respiratory failure – Benzodiazepines, including lorazepam, may depress central nervous system respiratory drive and are contraindicated in severe respiratory failure. An example would be the inappropriate use to relieve anxiety associated with acute severe asthma. The anxiolytic effects may also be detrimental to a patient's willingness and ability to fight for breath. However, if mechanical ventilationbecomes necessary, lorazepam may be used to facilitate deep sedation.
Acute intoxication – Lorazepam may interact synergistically with the effects of alcohol, narcotics, or other psychoactive substances. It should, therefore, not be administered to a drunk or intoxicated person.
Ataxia – This is a neurological clinical sign, consisting of unsteady and clumsy motion of the limbs and torso, due to the failure of gross muscle movement coordination, most evident on standing and walking. It is the classic way in which acute alcohol intoxication may affect a person. Benzodiazepines should not be administered to already-ataxic patients.
Acute narrow-angle glaucoma – Lorazepam has pupil-dilating effects, which may further interfere with the drainage of aqueous humor from the anterior chamber of the eye, thus worsening narrow-angle glaucoma.
Sleep apnea – Sleep apnea may be worsened by lorazepam's central nervous system depressant effects. It may further reduce the patient's ability to protect his or her airway during sleep.[57]
Myasthenia gravis – This condition is characterized by muscle weakness, so a muscle relaxant such as lorazepam may exacerbate symptoms.
Pregnancy and breastfeeding – Lorazepam belongs to the Food and Drug Administration (FDA) pregnancy category D, which means it is likely to cause harm to the developing baby if taken during the first trimester of pregnancy. The evidence is inconclusive whether lorazepam if taken early in pregnancy results in reduced intelligence, neurodevelopmental problems, physical malformations in cardiac or facial structure, or other malformations in some newborns. Lorazepam given to pregnant women antenatally may cause floppy infant syndrome[58] in the neonate, or respiratory depression necessitating ventilation. Regular lorazepam use during late pregnancy (the third trimester), carries a definite risk of benzodiazepine withdrawal syndrome in the neonate. Neonatal benzodiazepine withdrawal may include hypotonia, reluctance to suck, apneicspells, cyanosis, and impaired metabolic responses to cold stress. Symptoms of floppy infant syndrome and the neonatal benzodiazepine withdrawal syndrome have been reported to persist from hours to months after birth.[59] Lorazepam may also inhibit fetal liver bilirubin glucuronidation, leading to neonatal jaundice. Lorazepam is present in breast milk, so caution must be exercised about breastfeeding.
Specific groups
Children and the elderly – The safety and effectiveness of lorazepam is not well determined in children under 18 years of age, but it is used to treat acute seizures. Dose requirements have to be individualized, especially in the elderly and debilitated patients in whom the risk of oversedation is greater. Long-term therapy may lead to cognitive deficits, especially in the elderly, which may only be partially reversible. The elderly metabolize benzodiazepines more slowly than younger people and are more sensitive to the adverse effects of benzodiazepines compared to younger individuals even at similar plasma levels. Additionally, the elderly tend to take more drugs which may interact or enhance the effects of benzodiazepines. Benzodiazepines, including lorazepam, have been found to increase the risk of falls and fractures in the elderly. As a result, dosage recommendations for the elderly are about half of those used in younger individuals and used for no longer than two weeks.[9][60] Lorazepam may also be slower to clear in the elderly, leading potentially to accumulation and enhanced effects.[61] Lorazepam, similar to other benzodiazepines and nonbenzodiazepines, causes impairments in body balance and standing steadiness in individuals who wake up at night or the next morning. Falls and hip fractures are frequently reported. The combination with alcohol increases these impairments. Partial, but incomplete, tolerance develops to these impairments.[10]
Liver or kidney failure – Lorazepam may be safer than most benzodiazepines in patients with impaired liver function. Like oxazepam, it does not require hepatic oxidation, but only hepatic glucuronidation into lorazepam-glucuronide. Therefore, impaired liver function is unlikely to result in lorazepam accumulation to an extent causing adverse reactions.[26] Similarly renal disease has minimal effects on lorazepam levels.[62]
Surgical premedication – Informed consent given only after receiving lorazepam premedication could have its validity challenged later. Staff must use chaperones to guard against allegations of abuse during treatment. Such allegations may arise because of incomplete amnesia, disinhibition, and impaired ability to process cues. Because of its relative long duration of residual effects (sedation, ataxia, hypotension, and amnesia), lorazepam premedication is best suited for hospital inpatient use. Patients should not be discharged from the hospital within 24 hours of receiving lorazepam premedication unless accompanied by a caregiver. They should also not drive, operate machinery, or use alcohol within this period.
Drug and alcohol dependence – The risk of abuse of lorazepam is increased in dependent patients.[60]
Comorbid psychiatric disorders also increase the risk of dependence and paradoxical adverse effects.[60]
Tolerance and dependence
Dependence typified by a withdrawal syndrome occurs in about one-third of individuals who are treated for longer than four weeks with a benzodiazepine. Higher doses and longer periods of use increase the risk of developing a benzodiazepine dependence. Potent benzodiazepines, such as lorazepam, alprazolam, and triazolam, have the highest risk of causing a dependence.[9] Tolerance to benzodiazepine effects develops with regular use. This is desirable with amnesic and sedative effects but undesirable with anxiolytic, hypnotic, and anticonvulsant effects. Patients initially experience drastic relief from anxiety and sleeplessness, but symptoms gradually return, relatively soon in the case of insomnia, but more slowly in the case of anxiety symptoms. After four to six months of regular benzodiazepine use, evidence of continued efficacy declines.
If regular treatment is continued for longer than four to six months, dose increases may be necessary to maintain effects, but treatment-resistant symptoms may in fact be benzodiazepine withdrawal symptoms.[63] Due to the development of tolerance to the anticonvulsant effects, benzodiazepines are generally not recommended for long-term use for the management of epilepsy. Increasing the dose may overcome tolerance, but tolerance may then develop to the higher dose and adverse effects may persist and worsen. The mechanism of tolerance to benzodiazepines is complex and involves GABAA receptor downregulation, alterations to subunit configuration of GABAA receptors, uncouplingand internalisation of the benzodiazepine binding site from the GABAA receptor complex as well as changes in gene expression.[9]
The likelihood of dependence is relatively high with lorazepam compared to other benzodiazepines. Lorazepam's relatively short serum half-life, its confinement mainly to the vascular space, and its inactive metabolite can result in interdose withdrawal phenomena and next-dose cravings, that may reinforce psychological dependence. Because of its high potency, the smallest lorazepam tablet strength of 0.5 mg is also a significant dose reduction (in the UK, the smallest tablet strength is 1.0 mg, which further accentuates this difficulty). To minimise the risk of physical/psychological dependence, lorazepam is best used only short-term, at the smallest effective dose. If any benzodiazepine has been used long-term, the recommendation is a gradual dose taper over a period of weeks, months or longer, according to dose and duration of use, the degree of dependence and the individual.
Coming off long-term lorazepam use may be more realistically achieved by a gradual switch to an equivalent dose of diazepam and a period of stabilization on this, and only then initiating dose reductions. The advantage of switching to diazepam is that dose reductions are felt less acutely, because of the longer half-lives (20–200 hours) of diazepam and its active metabolites.[64]
Withdrawal
On abrupt or overly rapid discontinuation of lorazepam, anxiety, and signs of physical withdrawal have been observed, similar to those seen on withdrawal from alcohol and barbiturates. Lorazepam, as with other benzodiazepine drugs, can cause physical dependence, addiction, and benzodiazepine withdrawal syndrome. The higher the dose and the longer the drug is taken, the greater the risk of experiencing unpleasant withdrawal symptoms. Withdrawal symptoms can, however, occur from standard dosages and also after short-term use. Benzodiazepine treatment should be discontinued as soon as possible via a slow and gradual dose reduction regimen.[65] Rebound effects often resemble the condition being treated, but typically at a more intense level and may be difficult to diagnose. Withdrawal symptoms can range from mild anxiety and insomnia to more severe symptoms such as seizures and psychosis. The risk and severity of withdrawal are increased with long-term use, use of high doses, abrupt or over-rapid reduction, among other factors. Short-acting benzodiazepines such as lorazepam are more likely to cause a more severe withdrawal syndrome compared to longer-acting benzodiazepines.[9]
Withdrawal symptoms can occur after taking therapeutic doses of Ativan for as little as one week. Withdrawal symptoms include headaches, anxiety, tension, depression, insomnia, restlessness, confusion, irritability, sweating, dysphoria, dizziness, derealization, depersonalization, numbness/tingling of extremities, hypersensitivity to light, sound, and smell, perceptual distortions, nausea, vomiting, diarrhea, appetite loss, hallucinations, delirium, seizures, tremor, stomach cramps, myalgia, agitation, palpitations, tachycardia, panic attacks, short-term memory loss, and hyperthermia. It takes about 18–36 hours for the benzodiazepine to be removed from the body.[66] The ease of addiction to lorazepam, (Ativan brand was particularly cited), and its withdrawal were brought to the attention of the British public during the early 1980s in Esther Rantzen's BBC TV series That's Life!, in a feature on the drug over a number of episodes.
Interactions
Lorazepam is not usually fatal in overdose, but may cause fatal respiratory depression if taken in overdose with alcohol. The combination also causes synergistic enhancement of the disinhibitory and amnesic effects of both drugs, with potentially embarrassing or criminal consequences. Some experts advise that patients should be warned against drinking alcohol while on lorazepam treatment,[29][67] but such clear warnings are not universal.[68] Synergistic adverse effects may also occur when lorazepam is administered with other drugs, such as opioids or other hypnotics.[62] Lorazepam may also interact with rifabutin.[69] Valproate inhibits the metabolism of lorazepam, whereas carbamazepine, lamotrigine, phenobarbital, phenytoin, and rifampin increase its rate of metabolism. Some antidepressants, antiepileptic drugs such as phenobarbital, phenytoin and carbamazepine, sedative antihistamines, opiates, antipsychotics and alcohol, when taken with lorazepam may result in enhanced sedative effects.[9]
Adverse effects
Many beneficial effects of lorazepam (e.g., sedative, muscle relaxant, anti-anxiety, and amnesic effects) may become adverse effects when unwanted.[29] Adverse effects can include sedation and low blood pressure; the effects of lorazepam are increased in combination with other CNS depressant drugs.[21][35] Other adverse effects include confusion, ataxia, inhibiting the formation of new memories, and hangover effects. With long-term benzodiazepine use it is unclear whether cognitive impairments fully return to normal after stopping lorazepam use; cognitive deficits persist for at least six months after withdrawal, but longer than six months may be required for recovery of cognitive function. Lorazepam appears to have more profound adverse effects on memory than other benzodiazepines; it impairs both explicit and implicit memory.[43][44] In the elderly, falls may occur as a result of benzodiazepines. Adverse effects are more common in the elderly, and they appear at lower doses than in younger patients. Benzodiazepines can cause or worsen depression. Paradoxical effects can also occur, such as worsening of seizures, or paradoxical excitement; paradoxical excitement is more likely to occur in the elderly, children, those with a history of alcohol abuse, and in people with a history of aggression or anger problems.[9] Lorazepam's effects are dose-dependent, meaning the higher the dose, the stronger the effects (and side effects) will be. Using the smallest dose needed to achieve desired effects lessens the risk of adverse effects. Sedative drugs and sleeping pills, including lorazepam, have been associated with an increased risk of death.[45]
Sedation is the side effect people taking lorazepam most frequently report. In a group of around 3,500 patients treated for anxiety, the most common side effects complained of from lorazepam were sedation (15.9%), dizziness (6.9%), weakness (4.2%), and unsteadiness (3.4%). Side effects such as sedation and unsteadiness increased with age.[46] Cognitive impairment, behavioural disinhibition and respiratory depression as well as hypotension may also occur.[34][38]
Paradoxical effects: In some cases, paradoxical effects can occur with benzodiazepines, such as increased hostility, aggression, angry outbursts, and psychomotor agitation. These effects are seen more commonly with lorazepam than with other benzodiazepines.[47]Paradoxical effects are more likely to occur with higher doses, in patients with pre-existing personality disorders and those with a psychiatric illness. Frustrating stimuli may trigger such reactions, though the drug may have been prescribed to help the patient cope with such stress and frustration in the first place. As paradoxical effects appear to be dose-related, they usually subside on dose reduction or on complete withdrawal of lorazepam.[48][49][50][51][52][53]
Suicidality: Benzodiazepines are associated with increased risk of suicide, possibly due to disinhibition.[8] Higher dosages appear to confer greater risk.
Amnesic effects: Among benzodiazepines, lorazepam has relatively strong amnesic effects,[29][54] but patients soon develop tolerance to this with regular use. To avoid amnesia (or excess sedation) being a problem, the initial total daily lorazepam dose should not exceed 2 mg. This also applies to use for night sedation. Five participants in a sleep study were prescribed lorazepam 4 mg at night, and the next evening, three subjects unexpectedly volunteered memory gaps for parts of that day, an effect that subsided completely after two to three days' use.[55]Amnesic effects cannot be estimated from the degree of sedation present, since the two effects are unrelated.
High-dose or prolonged parenterally administered lorazepam is sometimes associated with propylene glycol poisoning.[34][56]
Overdose
In cases of a suspected lorazepam overdose, it is important to establish whether the patient is a regular user of lorazepam or other benzodiazepines since regular use causes tolerance to develop. Also, one must ascertain whether other substances were also ingested.
Signs of overdose range through mental confusion, dysarthria, paradoxical reactions, drowsiness, hypotonia, ataxia, hypotension, hypnotic state, coma, cardiovascular depression, respiratory depression, and death.
Early management of alert patients includes emetics, gastric lavage, and activated charcoal. Otherwise, management is by observation, including of vital signs, support and, only if necessary, considering the hazards of doing so, giving intravenous flumazenil.
Patients are ideally nursed in a kind, frustration-free environment, since, when given or taken in high doses, benzodiazepines are more likely to cause paradoxical reactions. If shown sympathy, even quite crudely feigned, patients may respond solicitously, but they may respond with disproportionate aggression to frustrating cues.[70] Opportunistic counseling has limited value here, as the patient is unlikely to recall this later, owing to drug-induced anterograde amnesia.