药品详情:
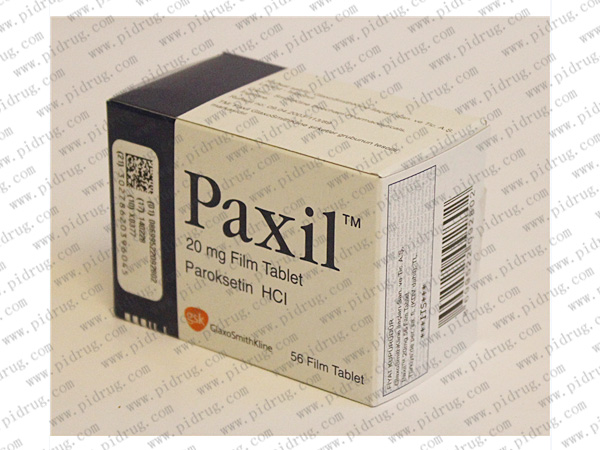
【帕罗西汀Paxil 简述】
帕罗西汀Paxil是一种苯基呃啶衍生物,是SSRI,可选择性地抑制5-HT转运体,阻断突触前膜对5-HT的再摄取, 延长和增加5-HT的作用,从而产生抗抑郁作用。
【帕罗西汀Paxil适应症】
①用于治疗抑郁症。适合治疗伴有焦虑症的抑郁症患者,作用比TCAs快,而且远期疗效比丙米嗪好。
②亦可用于原恐障碍、社交恐怖症及强迫症的治疗。
【帕罗西汀Paxil规格】
本品为片剂,每片含有效成份12.5mg/25mg,每瓶30片装。
【帕罗西汀Paxil服用方法】
由于剂型及规格不同,用法用量请仔细阅读药品说明书或遵医嘱。
【帕罗西汀Paxil注意事项】
①服用本药前后两周内不能使用 MA0Is。
②有癫痫或躁狂病史、闭角型青光眼、有出血倾向、有自杀倾向者或严重抑郁状态病史者慎用。肝、肾功能不全者仍可安全使用,但应降低剂量。
③一次性给药后,可出现轻微的心率减慢、血压波动,一般无临床意义,但对有心血管疾病或新发现有心肌梗死者,应注意其反应。
④服用1?3周后方可显效。用药时间足够长才可巩固疗效。抑郁症、强迫症、惊恐障碍的维持治疗期均较长。
⑤有报道迅速停药可引起综合征:睡眠障碍、激惹或焦虑、恶心、出汗、意识模糊。为避免停药反应,推荐撤药方案:根据患者耐受情况,如果能够耐受,以每周10mg的速度减量,至每日20mg的剂量应维持口服1周再停药。如果不能耐受可降低所减剂量,如患者反应强烈,则可考虑回复原剂量。
【帕罗西汀Paxil不良反应】
本品可引起轻微而短暂的不良反应。常见的有轻度口干、恶心、厌 食、便秘、头疼、震颤、乏力、失眠和性功能障碍。偶见神 经性水肿、荨麻疹、体位性低血压。罕见锥体外系反应的报道。
注:药品如有新包装,以新包装为准。以上资讯来源于网络或由高等医药院校的学生志愿者翻译(如有错漏,请帮忙指正),仅供医护人员内部讨论,不作任何用药依据,具体用药指引,请咨询主治医师。
如您发现本网站有文字编辑或内容错误,请点击此处发送(需要安装有foxmail或outlook支持),
或发邮件至:info@pidrug.com,香港济民药业感谢您的到访!
欢迎您添加香港济民药业微信,或在公众号内留言。